Gastric Bypass
Bariatric Surgery
Bariatric surgery is intended for people who are approximately 100 pounds or more overweight (with a Body Mass Index of 40 or greater) and who have not had success with other medical therapies such as diet, exercise, medications, etc. In some cases, a person with a Body Mass Index (BMI) of 35 or greater and one or more co-morbid conditions may be considered for bariatric surgery.
Roux-en-Y Gastric Bypass
- Small stomach pouch created.
- Bypass of small intestines, limiting the absorption of calories.
- Food is delayed in mixing with the bile and pancreatic juices that aid in the absorption of nutrients.
- Results in an early sense of fullness, combined with a sense of satisfaction. This reduces the desire to eat.
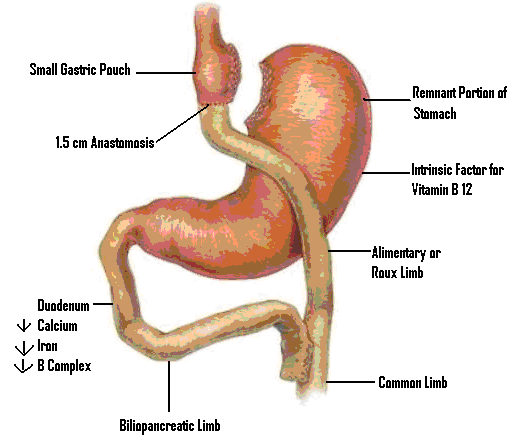
- The Roux-en-Y Gastric Bypass is one of the most frequently performed bariatric procedures in the United States. In this procedure, stapling creates a small stomach pouch.
- The remainder of the stomach is not removed, but it is divided from the newly created stomach. The outlet from the formed pouch empties directly into the upper portion of the jejunum, thus bypassing calorie absorption and the duodenum. This is done by dividing the small intestine just beyond the duodenum and constructing a connection with the new, smaller stomach pouch. The length of either segment of the intestine can be increased to produce lower or higher levels of malabsorption. The larger part of the stomach and duodenum are connected to the lower jejunum.
Advantages:
- Average weight loss in the Roux-en-Y procedure is generally higher in a compliant patient than with purely restrictive procedures.
- One year after surgery, weight loss can average 77% of excess body weight. (weight loss varies with individuals)
- Studies show that after 10-14 years, 60% of excess body weight loss has been maintained by patients. A 2004 meta-analysis of more than 22,000 patients showed that those who underwent a bariatric surgical procedure experienced complete remission or improvement of their co-morbid conditions including diabetes, hyperlipidemia, hypertension, and obstructive sleep apnea.
Risk:
The following are in addition to the general risks of surgery:
- Because the duodenum is bypassed, poor absorption of iron and calcium can result in the lowering of total body iron and cause a predisposition to iron deficiency anemia.
- Bypassing the duodenum has caused metabolic bone disease in some patients, resulting in bone pain, loss of height, humped back, and fractures of the ribs and hip bones. Women should be aware of the potential for heightened bone calcium loss. All of the deficiencies mentioned above, however, can be managed through proper diet and vitamin and mineral supplements.
- Chronic anemia due to vitamin B12 deficiency can occur. This can usually be managed with sublingual tablets, nasal spray or injections of vitamin B12.
- When removing or bypassing the pylorus, a condition known as “Dumping Syndrome” can occur as the result of rapid emptying of stomach contents into the small intestine. This is sometimes triggered when too much sugar or large amounts of food are consumed. While generally not considered a serious risk to your health, the result can be extremely unpleasant and can include nausea, weakness, sweating, faintness, and diarrhea after eating.
- In some cases, the effectiveness of the procedure may be reduced if the stomach pouch is stretched. Overeating can chronically stretch the pouch.
- The remnant stomach pouch and segments of the small intestine cannot be easily visualized using x-ray or endoscopy if problems such ulcers, bleeding, or malignancy should occur.
- Talk with the surgeon about the possible surgical risks.
Complications
As with any surgery, there are immediate and long-term complications. Possible risks can include, but are not limited to:
- Bleeding*
- Complications due to anesthesia and medications
- Deep vein thrombosis
- Pulmonary embolism
- Dehiscence (separation of areas that are stitched or stapled together)
- Infections
- Leaks from staple lines
- Marginal ulcers
- Spleen injury*
- Stenosis (narrowing of a passage, such as valve)
- Internal hernias
- Gallstones
- Changes in body image
- Death
*To control operative bleeding, removal of the spleen may be necessary.
